*In blount's disease, the knee is stable in full extension, but the medial femoral condyle may sublux posteromedially (into the depressed medial tibial plateau) at 10-20 degrees of flexion. This is called Siffert-katz sign.
*Tibia vara is otherwise called Blount's disease.
*The signs and symptoms of blount's disease are :
1. Intercondylar distance greater than 6 cms
2. Shot stature
3. Weight excessive for height
4. Severe deformity
5. Palpable metaphyseal beaking
6. Knee instability
7. Knee pain
8. Presence of Siffert-katz sign
---------------------------------------
Q: Presence of siffert-katz sign is a feature of ?
a. Blount's disease
b. cubitus varus
c. cubitus valgus
d. coxa valgus
answer: a. blount's disease.
p.s= This question was asked in the DNB december 2009 question paper.
Sunday, December 20, 2009
Thursday, December 17, 2009
63 - Akathisia
Akathisia, or acathisia, is a syndrome characterized by unpleasant sensations of "inner" restlessness that manifests itself with an inability to sit still or remain motionless (hence the word's origin in ancient Greek α (a), [without, not] + κάθισις (káthisis), [sitting]).
Its most common cause is as a side effect of medications, mainly neuroleptic antipsychotics especially the phenothiazines (such as perphenazine and chlorpromazine), thioxanthenes (such as flupenthixol and zuclopenthixol) and butyrophenones (such as haloperidol (Haldol)), piperazines (such as ziprasidone), antispasmodics (such as metoclopramide), and antidepressants. Akathisia can also, to a lesser extent, be caused by Parkinson's disease and related syndromes.
However, most antipsychotic psychotropic drugs cause Parkinsonian like symptoms due to blockage of dopamine receptors in the nigrostriatal pathway of the brain. Another major cause is the withdrawal from opioid medications.
Akathisia may range in intensity from a mild sense of disquiet or anxiety (which may be easily overlooked) to a total inability to sit still, accompanied by overwhelming anxiety, malaise, and severe dysphoria (manifesting as an almost indescribable sense of terror and doom).
The condition is difficult for the patient to describe and is often misdiagnosed. When misdiagnosis occurs in antipsychotic neuroleptic-induced akathisia, more antipsychotic neuroleptics may be prescribed, potentially worsening the symptoms.
High-functioning patients have described the feeling as a sense of inner tension and torment or chemical torture.
The presence and severity of akathisia can be measured using the Barnes Akathisia Scale.
Reports of akathisic states can be found in the medical literature before the advent of neuroleptics. Healy, et al. (2006), described the following regarding akathisia: tension, insomnia, a sense of discomfort, motor restlessness, and marked anxiety and panic. Increased labile affect can result, such as weepiness. Interestingly, in some people the opposite response to SSRIs occurs, in the form of emotional blunting; but sufficient clinical research has not yet been made in this area.
Jack Henry Abbot (1981) described the effects of akathisia produced by antipsychotic drugs:
These drugs, in this family, do not calm or sedate the nerves. They attack. They attack from so deep inside you, you cannot locate the source of the pain ... The muscles of your jawbone go berserk, so that you bite the inside of your mouth and your jaw locks and the pain throbs. For hours every day this will occur. Your spinal column stiffens so that you can hardly move your head or your neck and sometimes your back bends like a bow and you cannot stand up. The pain grinds into your fiber ... You ache with restlessness, so you feel you have to walk, to pace. And then as soon as you start pacing, the opposite occurs to you; you must sit and rest. Back and forth, up and down you go in pain you cannot locate, in such wretched anxiety you are overwhelmed, because you cannot get relief even in breathing.
—Jack Henry Abbot, In the Belly of the Beast (1981/1991). Vintage Books, 35–36. Quoted in Robert Whitaker, Mad in America (2002, ISBN 0738207993), 187.
Treatment non-compliance is a common consequence of neuroleptic-induced akathisia. At the extreme end of non-compliance, patients who have been treated with neuroleptic antipsychotics for psychotic episodes or prochlorperazine for nausea may rarely run away from hospitals or emergency rooms due to this disconcerting sensation.
CAUSES :
Akathisia is most often seen as a side effect of antipsychotic medications and medications such as reglan, but has other causes as well:
1.Non-sedating antipsychotics such as haloperidol (Haldol), droperidol, pimozide, trifluoperazine, amisulpride, risperidone, aripiprazole (Abilify) and asenapine (Saphris).
2.Less common in sedating antipsychotics such as zuclopenthixol (Cisordinol) or chlorpromazine where anticholinergic and antihistaminergic effects counteract akathisia to a degree.
3.SSRIs, such as fluoxetine (Prozac).[9] It has also been documented with the use of paroxetine (Paxil).Akathisia has been studied as the mechanism by which SSRI-induced suicidality occurs.
4.Other antidepressants, such as venlafaxine, the tricyclics and trazodone (Desyrel).
5.Certain anti-emetic drugs, particularly the dopamine blockers, such as metoclopramide (Reglan) and prochlorperazine (Compazine).
6.Opioid withdrawal.
The 2006 UK study by Healy, Herxheimer, and Menkes observed that akathisia is often miscoded in antidepressant clinical trials as "agitation, emotional lability, and hyperkinesis (overactivity)". The study further points out that misdiagnosis of akathisia as simple motor restlessness occurs, but that this is more properly classed as dyskinesia. Healy, et al., further show links between antidepressant-induced akathisia and violence, including suicide, as akathisia can "exacerbate psychopathology." The study goes on to state that there is extensive clinical evidence correlating akathisia with SSRI use, showing that approximately ten times as many patients on SSRIs as those on placebos showed symptoms severe enough to drop out of a trial (5.0% compared to 0.5%).
TREATMENT :
Acute akathisia is treated with medications, most often diphenhydramine (Benadryl). Teatment can also include the discontinuation or reduction of dose of the causative agent.
Akathisia can also be reduced by administering other drugs, though effectiveness can vary with more severe cases resistant to most drug treatment. Benzodiazepines like clonazepam (Klonopin) are effective. Some consider the drug of choice for the treatment of akathisia to be beta-blockers such as propranolol (Inderal) or metoprolol. The antihistamine cyproheptadine is also effective, though with shorter effect than beta blockers.
One study showed that vitamin B6 is effective for the treatment of neuroleptic-induced akathisia.
N Acetyl Cysteine also showed a positive effect on akathisia in an RCT.
Its most common cause is as a side effect of medications, mainly neuroleptic antipsychotics especially the phenothiazines (such as perphenazine and chlorpromazine), thioxanthenes (such as flupenthixol and zuclopenthixol) and butyrophenones (such as haloperidol (Haldol)), piperazines (such as ziprasidone), antispasmodics (such as metoclopramide), and antidepressants. Akathisia can also, to a lesser extent, be caused by Parkinson's disease and related syndromes.
However, most antipsychotic psychotropic drugs cause Parkinsonian like symptoms due to blockage of dopamine receptors in the nigrostriatal pathway of the brain. Another major cause is the withdrawal from opioid medications.
Akathisia may range in intensity from a mild sense of disquiet or anxiety (which may be easily overlooked) to a total inability to sit still, accompanied by overwhelming anxiety, malaise, and severe dysphoria (manifesting as an almost indescribable sense of terror and doom).
The condition is difficult for the patient to describe and is often misdiagnosed. When misdiagnosis occurs in antipsychotic neuroleptic-induced akathisia, more antipsychotic neuroleptics may be prescribed, potentially worsening the symptoms.
High-functioning patients have described the feeling as a sense of inner tension and torment or chemical torture.
The presence and severity of akathisia can be measured using the Barnes Akathisia Scale.
Reports of akathisic states can be found in the medical literature before the advent of neuroleptics. Healy, et al. (2006), described the following regarding akathisia: tension, insomnia, a sense of discomfort, motor restlessness, and marked anxiety and panic. Increased labile affect can result, such as weepiness. Interestingly, in some people the opposite response to SSRIs occurs, in the form of emotional blunting; but sufficient clinical research has not yet been made in this area.
Jack Henry Abbot (1981) described the effects of akathisia produced by antipsychotic drugs:
These drugs, in this family, do not calm or sedate the nerves. They attack. They attack from so deep inside you, you cannot locate the source of the pain ... The muscles of your jawbone go berserk, so that you bite the inside of your mouth and your jaw locks and the pain throbs. For hours every day this will occur. Your spinal column stiffens so that you can hardly move your head or your neck and sometimes your back bends like a bow and you cannot stand up. The pain grinds into your fiber ... You ache with restlessness, so you feel you have to walk, to pace. And then as soon as you start pacing, the opposite occurs to you; you must sit and rest. Back and forth, up and down you go in pain you cannot locate, in such wretched anxiety you are overwhelmed, because you cannot get relief even in breathing.
—Jack Henry Abbot, In the Belly of the Beast (1981/1991). Vintage Books, 35–36. Quoted in Robert Whitaker, Mad in America (2002, ISBN 0738207993), 187.
Treatment non-compliance is a common consequence of neuroleptic-induced akathisia. At the extreme end of non-compliance, patients who have been treated with neuroleptic antipsychotics for psychotic episodes or prochlorperazine for nausea may rarely run away from hospitals or emergency rooms due to this disconcerting sensation.
CAUSES :
Akathisia is most often seen as a side effect of antipsychotic medications and medications such as reglan, but has other causes as well:
1.Non-sedating antipsychotics such as haloperidol (Haldol), droperidol, pimozide, trifluoperazine, amisulpride, risperidone, aripiprazole (Abilify) and asenapine (Saphris).
2.Less common in sedating antipsychotics such as zuclopenthixol (Cisordinol) or chlorpromazine where anticholinergic and antihistaminergic effects counteract akathisia to a degree.
3.SSRIs, such as fluoxetine (Prozac).[9] It has also been documented with the use of paroxetine (Paxil).Akathisia has been studied as the mechanism by which SSRI-induced suicidality occurs.
4.Other antidepressants, such as venlafaxine, the tricyclics and trazodone (Desyrel).
5.Certain anti-emetic drugs, particularly the dopamine blockers, such as metoclopramide (Reglan) and prochlorperazine (Compazine).
6.Opioid withdrawal.
The 2006 UK study by Healy, Herxheimer, and Menkes observed that akathisia is often miscoded in antidepressant clinical trials as "agitation, emotional lability, and hyperkinesis (overactivity)". The study further points out that misdiagnosis of akathisia as simple motor restlessness occurs, but that this is more properly classed as dyskinesia. Healy, et al., further show links between antidepressant-induced akathisia and violence, including suicide, as akathisia can "exacerbate psychopathology." The study goes on to state that there is extensive clinical evidence correlating akathisia with SSRI use, showing that approximately ten times as many patients on SSRIs as those on placebos showed symptoms severe enough to drop out of a trial (5.0% compared to 0.5%).
TREATMENT :
Acute akathisia is treated with medications, most often diphenhydramine (Benadryl). Teatment can also include the discontinuation or reduction of dose of the causative agent.
Akathisia can also be reduced by administering other drugs, though effectiveness can vary with more severe cases resistant to most drug treatment. Benzodiazepines like clonazepam (Klonopin) are effective. Some consider the drug of choice for the treatment of akathisia to be beta-blockers such as propranolol (Inderal) or metoprolol. The antihistamine cyproheptadine is also effective, though with shorter effect than beta blockers.
One study showed that vitamin B6 is effective for the treatment of neuroleptic-induced akathisia.
N Acetyl Cysteine also showed a positive effect on akathisia in an RCT.
Saturday, December 12, 2009
62 - Muehrcke's lines
*Muehrcke's lines, or leukonychia striata, are changes in the fingernail that may be a sign of an underlying medical disorder or condition.
*Muehrcke's lines are white lines (leukonychia) that extend all the way across the nail and lie parallel to the lunula (half moon).
*In contrast to Beau's lines, they are not grooved. The lines are actually in the vascular nail bed underneath the nail plate, and as such, they do not move with nail growth.
*Meuhrcke's lines disappear when pressure is placed over the nail, blanching the underlying nail bed.
*The appearance of Muehrcke's lines is nonspecific, but they are often associated with decreased protein synthesis, which may occur during periods of metabolic stress (e.g., after chemotherapy) and in hypoalbuminemic states such as the nephrotic syndrome.
*An example of Muehrcke's lines in the context of chemotherapy was published in the New England Journal of Medicine in 2007.
*Muehrcke's lines were described by Robert C. Muehrcke in 1956.
Friday, December 11, 2009
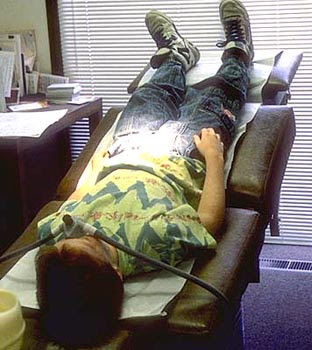
61 - Trendelenburg position
*In the Trendelenburg position the body is laid flat on the back (supine position) with the feet higher than the head, in contrast to the reverse Trendelenburg position, where the body is tilted in the opposite direction.
*Trendelenburg position is a standard position used in abdominal and gynecological surgery.
*It allows better access to the pelvic organs as gravity pulls the intestines away from the pelvis.
*It was named after the German surgeon Friedrich Trendelenburg.
USES OF TRENDELENBURG POSITION :
- Hypotensive patients (patients with low blood pressure) have historically been placed in the Trendelenburg position in hopes of increasing their cerebral perfusion pressure (the blood pressure in the brain). A 2005 literature review found the "Literature on the position was scarce, lacked strength, and seemed to be guided by 'expert opinion.' A 2008 review however found adverse consequences to the use of the Trendelenburg position and recommended it be avoided.However, the passive leg raising test is a useful clinical guide to fluid resuscitation and can be used for effective autotransfusion.
- The Trendelenburg position used to be the standard first aid position for shock.
- The Trendelenburg position was used for injured scuba divers. Many experienced divers still believe this position is appropriate, but current scuba first aid professionals no longer advocate elevating the feet higher than the head. The Trendelenburg position in this case increases regurgitation and airway problems, causes the brain to swell, increases breathing difficulty, and has not been proven to be of any value. "Supine is fine" is a good, general rule for victims of submersion injuries unless they have fluid in the airway or are breathing, in which case they should be positioned on the side.
- Perhaps because of its effect on breathing difficulty and airway problems, the Trendelenburg position is used in waterboarding. (Waterboarding is a form of torture that consists of immobilizing the victim on his or her back with the head inclined downwards, and then pouring water over the face and into the breathing passages, causing the captive to believe he or she is dying.)
- The Trendelenburg position may be used in childbirth when a woman's cervix is too swollen and won't quite dilate to 10 centimeters, or during the incidence of a prolapsed umbilical cord to take pressure off the cord and get more oxygen to the fetus, or it can be used to help rotate a posterior fetus either during pregnancy or the birth itself.
- Trendelenburg position in helpful in surgical reduction of an abdominal hernia.
- The Trendelenburg position is also used when placing a Central Venous Line. Trendelenburg position uses gravity to assist in the filling and distension of the upper central veins when placing a central line in the internal jugular or subclavian veins. It is also used in the placement of a external jugular peripheral line for the same reason. It plays no role in the placement of a femoral central venous line.
-----------------------------------------------------------
*Look at this question from the schwartz's principles of surgery (8th edition) - Self-assessment and board review :
Q: The initial treatment of a patient with a suspected air embolism includes which of the following ?
a. Place the patient in a right lateral decubitus position
b. Immediate angiographic aspiration of air
c. Place the patient in a trendelenburg position
d. Immediate thoractomy with pump stand-by
Answer : C.
Explanation :
- Several complications occur with central access lines involving a venous line or a pulmonary artery line .
- One such dangerous complication is the AIR EMBOLISM.
- It is estimated to occur in 0.2 to 1% of patients .
- However when an air embolism does occur, the results often can be dramatic and mortality can reach 50%.
- Treatment may prove futile if the diagnosis is ignored, especially if the air embolism bolus is larger than 50 mL.
- Clinical auscultation over the precordium is often non-specific, so a portable chest X-ray is required if the patient can tolerate the procedure.
- Nonetheless, aspiration via a central venous line accessing the heart may assist in decreasing the volume of gas in the right side of heart, and minimize the amount traversing into the pulmonary circulation.
- Maneuvers to entrap the air in the right heart include placing the patient in the LEFT LATERAL DECUBITUS position and in TRENDELENBURG POSITION, so the entrapped air can then be aspirated or anatomically stabilized within the right ventricle.
- If the patient survives these initial maneuvers, then consideration should be given as to whether the patient goes to the operating room for controlled surgical removal of the air, or if an angiographic approach is undertaken.
- The advantage of the operative approach is that the resources needed to salvage the patient are more readily available in the operating suite, should there be an acute deterioration in the patient's condition.
Tuesday, December 8, 2009
60 - Aprosexia, Hyperprosexia, Paraprosexia
Aprosexia, Hyperprosexia, and Paraprosexia are closely related medical and neuro-psychiatric phenomena associated with attention and concentration. They typically occurs in patients suffering traumatic brain injuries.
Aprosexia is an abnormal inability to pay attention, characterized by a near-complete indifference to everything.
Hyperprosexia is the abnormal state in which a person concentrates on one thing to the exclusion of everything else.
Paraprosexia is the inability to pay attention to any one thing (a state of constant distraction).
Patients suffering traumatic brain injury experience profound disturbance of the basic functions of the cognitive, behavioral, emotional and intellectual systems. Such patients' ability to regulate interaction between the ego and the external world is greatly diminished and they typically exhibit inflexible, concrete and sometimes inappropriate behaviors.
Aprosexia is an abnormal inability to pay attention, characterized by a near-complete indifference to everything.
Hyperprosexia is the abnormal state in which a person concentrates on one thing to the exclusion of everything else.
Paraprosexia is the inability to pay attention to any one thing (a state of constant distraction).
Patients suffering traumatic brain injury experience profound disturbance of the basic functions of the cognitive, behavioral, emotional and intellectual systems. Such patients' ability to regulate interaction between the ego and the external world is greatly diminished and they typically exhibit inflexible, concrete and sometimes inappropriate behaviors.
Subscribe to:
Posts (Atom)