*In blount's disease, the knee is stable in full extension, but the medial femoral condyle may sublux posteromedially (into the depressed medial tibial plateau) at 10-20 degrees of flexion. This is called Siffert-katz sign.
*Tibia vara is otherwise called Blount's disease.
*The signs and symptoms of blount's disease are :
1. Intercondylar distance greater than 6 cms
2. Shot stature
3. Weight excessive for height
4. Severe deformity
5. Palpable metaphyseal beaking
6. Knee instability
7. Knee pain
8. Presence of Siffert-katz sign
---------------------------------------
Q: Presence of siffert-katz sign is a feature of ?
a. Blount's disease
b. cubitus varus
c. cubitus valgus
d. coxa valgus
answer: a. blount's disease.
p.s= This question was asked in the DNB december 2009 question paper.
Sunday, December 20, 2009
Thursday, December 17, 2009
63 - Akathisia
Akathisia, or acathisia, is a syndrome characterized by unpleasant sensations of "inner" restlessness that manifests itself with an inability to sit still or remain motionless (hence the word's origin in ancient Greek α (a), [without, not] + κάθισις (káthisis), [sitting]).
Its most common cause is as a side effect of medications, mainly neuroleptic antipsychotics especially the phenothiazines (such as perphenazine and chlorpromazine), thioxanthenes (such as flupenthixol and zuclopenthixol) and butyrophenones (such as haloperidol (Haldol)), piperazines (such as ziprasidone), antispasmodics (such as metoclopramide), and antidepressants. Akathisia can also, to a lesser extent, be caused by Parkinson's disease and related syndromes.
However, most antipsychotic psychotropic drugs cause Parkinsonian like symptoms due to blockage of dopamine receptors in the nigrostriatal pathway of the brain. Another major cause is the withdrawal from opioid medications.
Akathisia may range in intensity from a mild sense of disquiet or anxiety (which may be easily overlooked) to a total inability to sit still, accompanied by overwhelming anxiety, malaise, and severe dysphoria (manifesting as an almost indescribable sense of terror and doom).
The condition is difficult for the patient to describe and is often misdiagnosed. When misdiagnosis occurs in antipsychotic neuroleptic-induced akathisia, more antipsychotic neuroleptics may be prescribed, potentially worsening the symptoms.
High-functioning patients have described the feeling as a sense of inner tension and torment or chemical torture.
The presence and severity of akathisia can be measured using the Barnes Akathisia Scale.
Reports of akathisic states can be found in the medical literature before the advent of neuroleptics. Healy, et al. (2006), described the following regarding akathisia: tension, insomnia, a sense of discomfort, motor restlessness, and marked anxiety and panic. Increased labile affect can result, such as weepiness. Interestingly, in some people the opposite response to SSRIs occurs, in the form of emotional blunting; but sufficient clinical research has not yet been made in this area.
Jack Henry Abbot (1981) described the effects of akathisia produced by antipsychotic drugs:
These drugs, in this family, do not calm or sedate the nerves. They attack. They attack from so deep inside you, you cannot locate the source of the pain ... The muscles of your jawbone go berserk, so that you bite the inside of your mouth and your jaw locks and the pain throbs. For hours every day this will occur. Your spinal column stiffens so that you can hardly move your head or your neck and sometimes your back bends like a bow and you cannot stand up. The pain grinds into your fiber ... You ache with restlessness, so you feel you have to walk, to pace. And then as soon as you start pacing, the opposite occurs to you; you must sit and rest. Back and forth, up and down you go in pain you cannot locate, in such wretched anxiety you are overwhelmed, because you cannot get relief even in breathing.
—Jack Henry Abbot, In the Belly of the Beast (1981/1991). Vintage Books, 35–36. Quoted in Robert Whitaker, Mad in America (2002, ISBN 0738207993), 187.
Treatment non-compliance is a common consequence of neuroleptic-induced akathisia. At the extreme end of non-compliance, patients who have been treated with neuroleptic antipsychotics for psychotic episodes or prochlorperazine for nausea may rarely run away from hospitals or emergency rooms due to this disconcerting sensation.
CAUSES :
Akathisia is most often seen as a side effect of antipsychotic medications and medications such as reglan, but has other causes as well:
1.Non-sedating antipsychotics such as haloperidol (Haldol), droperidol, pimozide, trifluoperazine, amisulpride, risperidone, aripiprazole (Abilify) and asenapine (Saphris).
2.Less common in sedating antipsychotics such as zuclopenthixol (Cisordinol) or chlorpromazine where anticholinergic and antihistaminergic effects counteract akathisia to a degree.
3.SSRIs, such as fluoxetine (Prozac).[9] It has also been documented with the use of paroxetine (Paxil).Akathisia has been studied as the mechanism by which SSRI-induced suicidality occurs.
4.Other antidepressants, such as venlafaxine, the tricyclics and trazodone (Desyrel).
5.Certain anti-emetic drugs, particularly the dopamine blockers, such as metoclopramide (Reglan) and prochlorperazine (Compazine).
6.Opioid withdrawal.
The 2006 UK study by Healy, Herxheimer, and Menkes observed that akathisia is often miscoded in antidepressant clinical trials as "agitation, emotional lability, and hyperkinesis (overactivity)". The study further points out that misdiagnosis of akathisia as simple motor restlessness occurs, but that this is more properly classed as dyskinesia. Healy, et al., further show links between antidepressant-induced akathisia and violence, including suicide, as akathisia can "exacerbate psychopathology." The study goes on to state that there is extensive clinical evidence correlating akathisia with SSRI use, showing that approximately ten times as many patients on SSRIs as those on placebos showed symptoms severe enough to drop out of a trial (5.0% compared to 0.5%).
TREATMENT :
Acute akathisia is treated with medications, most often diphenhydramine (Benadryl). Teatment can also include the discontinuation or reduction of dose of the causative agent.
Akathisia can also be reduced by administering other drugs, though effectiveness can vary with more severe cases resistant to most drug treatment. Benzodiazepines like clonazepam (Klonopin) are effective. Some consider the drug of choice for the treatment of akathisia to be beta-blockers such as propranolol (Inderal) or metoprolol. The antihistamine cyproheptadine is also effective, though with shorter effect than beta blockers.
One study showed that vitamin B6 is effective for the treatment of neuroleptic-induced akathisia.
N Acetyl Cysteine also showed a positive effect on akathisia in an RCT.
Its most common cause is as a side effect of medications, mainly neuroleptic antipsychotics especially the phenothiazines (such as perphenazine and chlorpromazine), thioxanthenes (such as flupenthixol and zuclopenthixol) and butyrophenones (such as haloperidol (Haldol)), piperazines (such as ziprasidone), antispasmodics (such as metoclopramide), and antidepressants. Akathisia can also, to a lesser extent, be caused by Parkinson's disease and related syndromes.
However, most antipsychotic psychotropic drugs cause Parkinsonian like symptoms due to blockage of dopamine receptors in the nigrostriatal pathway of the brain. Another major cause is the withdrawal from opioid medications.
Akathisia may range in intensity from a mild sense of disquiet or anxiety (which may be easily overlooked) to a total inability to sit still, accompanied by overwhelming anxiety, malaise, and severe dysphoria (manifesting as an almost indescribable sense of terror and doom).
The condition is difficult for the patient to describe and is often misdiagnosed. When misdiagnosis occurs in antipsychotic neuroleptic-induced akathisia, more antipsychotic neuroleptics may be prescribed, potentially worsening the symptoms.
High-functioning patients have described the feeling as a sense of inner tension and torment or chemical torture.
The presence and severity of akathisia can be measured using the Barnes Akathisia Scale.
Reports of akathisic states can be found in the medical literature before the advent of neuroleptics. Healy, et al. (2006), described the following regarding akathisia: tension, insomnia, a sense of discomfort, motor restlessness, and marked anxiety and panic. Increased labile affect can result, such as weepiness. Interestingly, in some people the opposite response to SSRIs occurs, in the form of emotional blunting; but sufficient clinical research has not yet been made in this area.
Jack Henry Abbot (1981) described the effects of akathisia produced by antipsychotic drugs:
These drugs, in this family, do not calm or sedate the nerves. They attack. They attack from so deep inside you, you cannot locate the source of the pain ... The muscles of your jawbone go berserk, so that you bite the inside of your mouth and your jaw locks and the pain throbs. For hours every day this will occur. Your spinal column stiffens so that you can hardly move your head or your neck and sometimes your back bends like a bow and you cannot stand up. The pain grinds into your fiber ... You ache with restlessness, so you feel you have to walk, to pace. And then as soon as you start pacing, the opposite occurs to you; you must sit and rest. Back and forth, up and down you go in pain you cannot locate, in such wretched anxiety you are overwhelmed, because you cannot get relief even in breathing.
—Jack Henry Abbot, In the Belly of the Beast (1981/1991). Vintage Books, 35–36. Quoted in Robert Whitaker, Mad in America (2002, ISBN 0738207993), 187.
Treatment non-compliance is a common consequence of neuroleptic-induced akathisia. At the extreme end of non-compliance, patients who have been treated with neuroleptic antipsychotics for psychotic episodes or prochlorperazine for nausea may rarely run away from hospitals or emergency rooms due to this disconcerting sensation.
CAUSES :
Akathisia is most often seen as a side effect of antipsychotic medications and medications such as reglan, but has other causes as well:
1.Non-sedating antipsychotics such as haloperidol (Haldol), droperidol, pimozide, trifluoperazine, amisulpride, risperidone, aripiprazole (Abilify) and asenapine (Saphris).
2.Less common in sedating antipsychotics such as zuclopenthixol (Cisordinol) or chlorpromazine where anticholinergic and antihistaminergic effects counteract akathisia to a degree.
3.SSRIs, such as fluoxetine (Prozac).[9] It has also been documented with the use of paroxetine (Paxil).Akathisia has been studied as the mechanism by which SSRI-induced suicidality occurs.
4.Other antidepressants, such as venlafaxine, the tricyclics and trazodone (Desyrel).
5.Certain anti-emetic drugs, particularly the dopamine blockers, such as metoclopramide (Reglan) and prochlorperazine (Compazine).
6.Opioid withdrawal.
The 2006 UK study by Healy, Herxheimer, and Menkes observed that akathisia is often miscoded in antidepressant clinical trials as "agitation, emotional lability, and hyperkinesis (overactivity)". The study further points out that misdiagnosis of akathisia as simple motor restlessness occurs, but that this is more properly classed as dyskinesia. Healy, et al., further show links between antidepressant-induced akathisia and violence, including suicide, as akathisia can "exacerbate psychopathology." The study goes on to state that there is extensive clinical evidence correlating akathisia with SSRI use, showing that approximately ten times as many patients on SSRIs as those on placebos showed symptoms severe enough to drop out of a trial (5.0% compared to 0.5%).
TREATMENT :
Acute akathisia is treated with medications, most often diphenhydramine (Benadryl). Teatment can also include the discontinuation or reduction of dose of the causative agent.
Akathisia can also be reduced by administering other drugs, though effectiveness can vary with more severe cases resistant to most drug treatment. Benzodiazepines like clonazepam (Klonopin) are effective. Some consider the drug of choice for the treatment of akathisia to be beta-blockers such as propranolol (Inderal) or metoprolol. The antihistamine cyproheptadine is also effective, though with shorter effect than beta blockers.
One study showed that vitamin B6 is effective for the treatment of neuroleptic-induced akathisia.
N Acetyl Cysteine also showed a positive effect on akathisia in an RCT.
Saturday, December 12, 2009
62 - Muehrcke's lines
*Muehrcke's lines, or leukonychia striata, are changes in the fingernail that may be a sign of an underlying medical disorder or condition.
*Muehrcke's lines are white lines (leukonychia) that extend all the way across the nail and lie parallel to the lunula (half moon).
*In contrast to Beau's lines, they are not grooved. The lines are actually in the vascular nail bed underneath the nail plate, and as such, they do not move with nail growth.
*Meuhrcke's lines disappear when pressure is placed over the nail, blanching the underlying nail bed.
*The appearance of Muehrcke's lines is nonspecific, but they are often associated with decreased protein synthesis, which may occur during periods of metabolic stress (e.g., after chemotherapy) and in hypoalbuminemic states such as the nephrotic syndrome.
*An example of Muehrcke's lines in the context of chemotherapy was published in the New England Journal of Medicine in 2007.
*Muehrcke's lines were described by Robert C. Muehrcke in 1956.
Friday, December 11, 2009
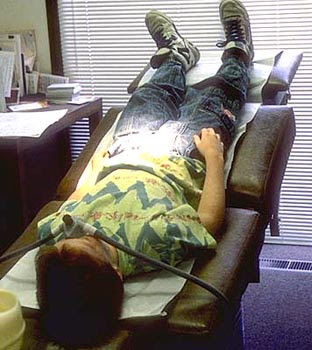
61 - Trendelenburg position
*In the Trendelenburg position the body is laid flat on the back (supine position) with the feet higher than the head, in contrast to the reverse Trendelenburg position, where the body is tilted in the opposite direction.
*Trendelenburg position is a standard position used in abdominal and gynecological surgery.
*It allows better access to the pelvic organs as gravity pulls the intestines away from the pelvis.
*It was named after the German surgeon Friedrich Trendelenburg.
USES OF TRENDELENBURG POSITION :
- Hypotensive patients (patients with low blood pressure) have historically been placed in the Trendelenburg position in hopes of increasing their cerebral perfusion pressure (the blood pressure in the brain). A 2005 literature review found the "Literature on the position was scarce, lacked strength, and seemed to be guided by 'expert opinion.' A 2008 review however found adverse consequences to the use of the Trendelenburg position and recommended it be avoided.However, the passive leg raising test is a useful clinical guide to fluid resuscitation and can be used for effective autotransfusion.
- The Trendelenburg position used to be the standard first aid position for shock.
- The Trendelenburg position was used for injured scuba divers. Many experienced divers still believe this position is appropriate, but current scuba first aid professionals no longer advocate elevating the feet higher than the head. The Trendelenburg position in this case increases regurgitation and airway problems, causes the brain to swell, increases breathing difficulty, and has not been proven to be of any value. "Supine is fine" is a good, general rule for victims of submersion injuries unless they have fluid in the airway or are breathing, in which case they should be positioned on the side.
- Perhaps because of its effect on breathing difficulty and airway problems, the Trendelenburg position is used in waterboarding. (Waterboarding is a form of torture that consists of immobilizing the victim on his or her back with the head inclined downwards, and then pouring water over the face and into the breathing passages, causing the captive to believe he or she is dying.)
- The Trendelenburg position may be used in childbirth when a woman's cervix is too swollen and won't quite dilate to 10 centimeters, or during the incidence of a prolapsed umbilical cord to take pressure off the cord and get more oxygen to the fetus, or it can be used to help rotate a posterior fetus either during pregnancy or the birth itself.
- Trendelenburg position in helpful in surgical reduction of an abdominal hernia.
- The Trendelenburg position is also used when placing a Central Venous Line. Trendelenburg position uses gravity to assist in the filling and distension of the upper central veins when placing a central line in the internal jugular or subclavian veins. It is also used in the placement of a external jugular peripheral line for the same reason. It plays no role in the placement of a femoral central venous line.
-----------------------------------------------------------
*Look at this question from the schwartz's principles of surgery (8th edition) - Self-assessment and board review :
Q: The initial treatment of a patient with a suspected air embolism includes which of the following ?
a. Place the patient in a right lateral decubitus position
b. Immediate angiographic aspiration of air
c. Place the patient in a trendelenburg position
d. Immediate thoractomy with pump stand-by
Answer : C.
Explanation :
- Several complications occur with central access lines involving a venous line or a pulmonary artery line .
- One such dangerous complication is the AIR EMBOLISM.
- It is estimated to occur in 0.2 to 1% of patients .
- However when an air embolism does occur, the results often can be dramatic and mortality can reach 50%.
- Treatment may prove futile if the diagnosis is ignored, especially if the air embolism bolus is larger than 50 mL.
- Clinical auscultation over the precordium is often non-specific, so a portable chest X-ray is required if the patient can tolerate the procedure.
- Nonetheless, aspiration via a central venous line accessing the heart may assist in decreasing the volume of gas in the right side of heart, and minimize the amount traversing into the pulmonary circulation.
- Maneuvers to entrap the air in the right heart include placing the patient in the LEFT LATERAL DECUBITUS position and in TRENDELENBURG POSITION, so the entrapped air can then be aspirated or anatomically stabilized within the right ventricle.
- If the patient survives these initial maneuvers, then consideration should be given as to whether the patient goes to the operating room for controlled surgical removal of the air, or if an angiographic approach is undertaken.
- The advantage of the operative approach is that the resources needed to salvage the patient are more readily available in the operating suite, should there be an acute deterioration in the patient's condition.
Tuesday, December 8, 2009
60 - Aprosexia, Hyperprosexia, Paraprosexia
Aprosexia, Hyperprosexia, and Paraprosexia are closely related medical and neuro-psychiatric phenomena associated with attention and concentration. They typically occurs in patients suffering traumatic brain injuries.
Aprosexia is an abnormal inability to pay attention, characterized by a near-complete indifference to everything.
Hyperprosexia is the abnormal state in which a person concentrates on one thing to the exclusion of everything else.
Paraprosexia is the inability to pay attention to any one thing (a state of constant distraction).
Patients suffering traumatic brain injury experience profound disturbance of the basic functions of the cognitive, behavioral, emotional and intellectual systems. Such patients' ability to regulate interaction between the ego and the external world is greatly diminished and they typically exhibit inflexible, concrete and sometimes inappropriate behaviors.
Aprosexia is an abnormal inability to pay attention, characterized by a near-complete indifference to everything.
Hyperprosexia is the abnormal state in which a person concentrates on one thing to the exclusion of everything else.
Paraprosexia is the inability to pay attention to any one thing (a state of constant distraction).
Patients suffering traumatic brain injury experience profound disturbance of the basic functions of the cognitive, behavioral, emotional and intellectual systems. Such patients' ability to regulate interaction between the ego and the external world is greatly diminished and they typically exhibit inflexible, concrete and sometimes inappropriate behaviors.
Thursday, October 22, 2009
59 - Botryomycosis
Botryomycosis; also known as bacterial pseudomycosis is a rare chronic granulomatous bacterial infection that affects the skin, and sometimes the viscera.
Botryomycosis has been known to affect humans, horses, cattle and swine.
The disease was originally discovered by Otto Bollinger (1843-1909) in 1870, and its name was coined by Sebastiano Rivolta (1832-1893) in 1884. The name refers to its grape-like granules (Gr. botryo = grapes) and the mistakenly implied fungal etiology (Gr. mykes = fungus). In 1919 the bacterial origin of the infection was discovered.
Staphylococcus aureus is usually the organism that causes the infection, however it can also be caused by Pseudomonas aeruginosa or several other species of bacteria. The anatomic structure of its lesion is similar to that of actinomycosis and mycetoma, and its granules resemble the sulfur granules of actinomycosis.
There are only a handful of documented cases of botryomycosis in humans, and its pathogenesis is not completely understood. However, it is usually described in individuals with impaired immunity, or with an underlying disease such as diabetes mellitus, cystic fibrosis or HIV infection.
Botryomycosis has been known to affect humans, horses, cattle and swine.
The disease was originally discovered by Otto Bollinger (1843-1909) in 1870, and its name was coined by Sebastiano Rivolta (1832-1893) in 1884. The name refers to its grape-like granules (Gr. botryo = grapes) and the mistakenly implied fungal etiology (Gr. mykes = fungus). In 1919 the bacterial origin of the infection was discovered.
Staphylococcus aureus is usually the organism that causes the infection, however it can also be caused by Pseudomonas aeruginosa or several other species of bacteria. The anatomic structure of its lesion is similar to that of actinomycosis and mycetoma, and its granules resemble the sulfur granules of actinomycosis.
There are only a handful of documented cases of botryomycosis in humans, and its pathogenesis is not completely understood. However, it is usually described in individuals with impaired immunity, or with an underlying disease such as diabetes mellitus, cystic fibrosis or HIV infection.
Tuesday, October 13, 2009
58 - Mermaid syndrome (Mermaid baby) (sirenomelia)
Sirenomelia, alternatively known as mermaid syndrome is a very rare congenital deformity in which the legs are fused together, giving the appearance of a mermaid's tail.
This condition is found in approximately one out of every 100,000 live births(about as rare as conjoined twins) and is usually fatal within a day or two of birth because of complications associated with abnormal kidney and bladder development and function. More than half the cases of sirenomelia result in stillbirth and this condition is 100 times more likely to occur in identical twins than in single births or fraternal twins. It results from a failure of normal vascular supply from the lower aorta in utero. Maternal diabetes has been associated with caudal regression syndrome and sirenomelia, although this association is not generally accepted. Intake of HALOPERIDOL during pregnancy is considered as one of the etiologies of sirenomelia.
VACTERL-H is an expanded form of the VACTERL association that concludes that this diagnosis is a less severe form of sirenomelia. The disorder was formerly thought to be an extreme case of Caudal regression syndrome; however, it was reclassified to be considered a separate condition.
Notable cases
Only a handful of patients who did not have the usual kidney and bladder complications have survived this condition, three of them being:
Milagros Cerrón
Milagros Cerrón Arauco (born April 27, 2004, in Huancayo, Peru). Although most of Milagros’ internal organs, including her heart and lungs, are in perfect condition, she was born with serious internal defects, including a deformed left kidney and a very small right one located very low in her body. In addition, her digestive, urinary tracts and genitals share a single tube. This birth defect occurs during the gastrulation week (week 3) of embryological development. Gastrulation establishes the three derm layers: ectoderm, mesoderm and endoderm. It seems that complications such as defects in the urogenital system as mentioned above can be possibly due to malformations in the intermediate mesoderm.
A four-hour operation to insert silicone bags between her legs to stretch the skin was successfully completed on February 8, 2005. A successful operation to separate her legs to just above the knee took place May 31, 2005, in a "Solidarity Hospital" in the district of Surquillo in Lima. The procedure, however, was so intensive that she became traumatized to the degree of losing her ability to form proper speech patterns, leaving her nearly mute. As yet it is not known if this is a physiological or psychological condition. However, at Milagros's second birthday, her mother reported that she knew more than 50 words. A second operation to complete the separation up to the groin took place on September 7, 2006. A few weeks later, she took her first steps.
Her doctor Luis Rubio said he was pleased with the progress Milagros had made, but cautioned that she still needed 10 to 15 years of rehabilitation and more operations before she could lead a normal life. Particularly, she will require reconstructive surgery to rebuild her rudimentary anus, urethra and genitalia.
Milagros' parents are from a poor village in Peru's Andes Mountains; the Solidarity Hospital has given a job to her father Ricardo Cerrón so that the family can remain in Lima, while the City of Lima has pledged to pay for many of the operations.
Tiffany Yorks
Tiffany Yorks of the United States (born May 7, 1988) underwent successful surgery in order to separate her legs. Her legs were successfully separated before she was one year old.She is the longest-surviving sirenomelia patient to date.
Shiloh Pepin
Shiloh Pepin was born in Kennebunkport, Maine in August, 1999, with her lower extremities fused, a missing bladder, uterus, colon and vagina, with only one partial kidney and one ovary. Her parents initially anticipated she could expect only a few months of life. An initial kidney transplant at 4 months of age, lasted a number of years, and in 2007 a second kidney transplant was successful. She attends Consolidated Elementary School. Shiloh is the only one of the three survivors of sirenomelia without surgery for separation of the conjoined legs.
Wednesday, October 7, 2009
57 - Sezary cell
*Sézary cells are medium to large lymphocytes with ceribriform nuclei and scant cytoplasm. The nucleus has been said to resemble a monocyte nucleus.
*An atypical T lymphocyte that contains vacuoles filled with mucopolysaccharide.
*It is a characteristic finding in cutaneous T-cell lymphoma and its variants and present in the peripheral blood of patients with Sézary syndrome. Clusters of these cells in the epidermis is called Pautrier's microabscess.
*Also known as:
-Pautrier's abscess
-Lutzner's cells
-Sézary-Lutzner cells.
Friday, August 14, 2009
56 - Giovanetti diet
A diet designed for patients with renal failure; it provides small amounts of protein, primarily as essential amino acids, along with alpha-keto derivatives of amino acids; breakdown of protein in skeletal muscle is retarded and, because transaminase reactions are reversible, a small proportion of the ammonia released by urea breakdown is used for synthesis of nonessential amino acids.
In patients with ARF, endogenous urea can be converted to non-essential aminoacids if an adequate amount of carbohydrate is provided. The Giordano Giovanetti diet contains a high carbbohydrate diet with limited protein. the use of commercially available essential aminoacids with hypertonic glucose aids control of electrolyte balance, lowers blood urea nitrogen levels, decreases the need for dialysis and speeds recovery of patients with acute tubular necrosis. Using high concentrations of glucose in a small volume allows even an oliguric patient to receive enough calories.
Feinstein employed an interesting approach to providing aminoacids to patients to hemodialysis-dependent renal failure by including them in diasylate .
In patients with ARF, endogenous urea can be converted to non-essential aminoacids if an adequate amount of carbohydrate is provided. The Giordano Giovanetti diet contains a high carbbohydrate diet with limited protein. the use of commercially available essential aminoacids with hypertonic glucose aids control of electrolyte balance, lowers blood urea nitrogen levels, decreases the need for dialysis and speeds recovery of patients with acute tubular necrosis. Using high concentrations of glucose in a small volume allows even an oliguric patient to receive enough calories.
Feinstein employed an interesting approach to providing aminoacids to patients to hemodialysis-dependent renal failure by including them in diasylate .
Saturday, June 13, 2009
55 - Sherrington law of reciprocal innervation
During the initiation of an eye movement, increased innervation to an extraocular muscle is accompanied by simultaneous inhibition ( a reciprocal decrease in innervation ) of the direct antagonist of the contracting muscle of the same eye.
If the left medial rectus muscle receives innervational flow to initiate adduction of the left eye, there is simultaneous decreased and inhibitory flow to the left lateral rectus muscle to make it relax and enable the eyeball to move medially.
If the left medial rectus muscle receives innervational flow to initiate adduction of the left eye, there is simultaneous decreased and inhibitory flow to the left lateral rectus muscle to make it relax and enable the eyeball to move medially.
Tuesday, June 2, 2009
54 - Reinke's crystals, Reinke's space and Reinke's oedema
Reinke's crystals are rod-shaped crystals in the interstitial cells of the testis and hilus cells of the ovary .
Reinke's space is seen in chronic laryngitis with swelling of the membranous part of the vocal cords .
This swelling of the vocal cords due to edema is also called Reinke's edema .
These are named after Friedrich Berthold Reinke ( 1862-1919 ), who was an anatomist from France .
1q: What is Reinke’s Oedema?
Reinke’s Oedema is a fluid filled swelling of one or both of the vocal cords.
The quality of the voice is likely to be affected by Reinke’s Oedema. Speaking may become more difficult and sound breathy or rough. The pitch of the voice may sound lower than it used to. These changes can be gradual.
2q: Causes and risks :
Reinke’s Oedema is most commonly associated with smoking. Some research shows a link with acid reflux and an under-active thyroid. It tends to affect women more than men.
3q: Diagnosing Reinke’s Oedema :
Usually an Ear Nose and Throat (ENT) doctor will examine the larynx (voice box) using a small flexible camera which goes through the nose ( flexible laryngoscope ) . This takes place in the outpatient’s clinic and does not require admission to hospital.If the ENT doctor suspects that an under-active thyroid is the cause of Reinke’s Oedema, they will arrange the appropriate tests.
4q: Treatments available :
The choice of treatment depends on the cause of Reinke’s Oedema.
• Surgery may be required to remove some of the fluid from the vocal cords.
• Speech and language therapy can help to improve vocal health and voice quality. speech and language therapist explains how to care for the voice and reduce vocal misuse and irritants.
• Medication to reduce acid reflux or balance the hormones produced by the thyroid gland if needed.
• Stopping smoking alone may result in Reinke’s Oedema subsiding.
5q: What a patient can do :
Looking after your voice, stopping smoking and reducing irritants can help the vocal cords to recover. Advice on how to do this will be given to you by the speech and language therapist. Advice sheets that are given to you should only be used under the direction and supervision of a qualified Speech and Language Therapist
If you continue to smoke and irritate your vocal cords after treatment, Reinke’s Oedema is likely to return.
Reinke's space is seen in chronic laryngitis with swelling of the membranous part of the vocal cords .
This swelling of the vocal cords due to edema is also called Reinke's edema .
These are named after Friedrich Berthold Reinke ( 1862-1919 ), who was an anatomist from France .
1q: What is Reinke’s Oedema?
Reinke’s Oedema is a fluid filled swelling of one or both of the vocal cords.
The quality of the voice is likely to be affected by Reinke’s Oedema. Speaking may become more difficult and sound breathy or rough. The pitch of the voice may sound lower than it used to. These changes can be gradual.
2q: Causes and risks :
Reinke’s Oedema is most commonly associated with smoking. Some research shows a link with acid reflux and an under-active thyroid. It tends to affect women more than men.
3q: Diagnosing Reinke’s Oedema :
Usually an Ear Nose and Throat (ENT) doctor will examine the larynx (voice box) using a small flexible camera which goes through the nose ( flexible laryngoscope ) . This takes place in the outpatient’s clinic and does not require admission to hospital.If the ENT doctor suspects that an under-active thyroid is the cause of Reinke’s Oedema, they will arrange the appropriate tests.
4q: Treatments available :
The choice of treatment depends on the cause of Reinke’s Oedema.
• Surgery may be required to remove some of the fluid from the vocal cords.
• Speech and language therapy can help to improve vocal health and voice quality. speech and language therapist explains how to care for the voice and reduce vocal misuse and irritants.
• Medication to reduce acid reflux or balance the hormones produced by the thyroid gland if needed.
• Stopping smoking alone may result in Reinke’s Oedema subsiding.
5q: What a patient can do :
Looking after your voice, stopping smoking and reducing irritants can help the vocal cords to recover. Advice on how to do this will be given to you by the speech and language therapist. Advice sheets that are given to you should only be used under the direction and supervision of a qualified Speech and Language Therapist
If you continue to smoke and irritate your vocal cords after treatment, Reinke’s Oedema is likely to return.
Saturday, May 2, 2009
53 - Lues maligna
While most HIV-infected individuals with syphilis have a typical presentation, a variety of formerly rare clinical problems may be encountered in the setting of dual infection .
Among them are lues maligna , an ulcerating lesion of the skin due to necrotizing vasculitis; unexplained fever; nephrotic syndrome and neurosyphilis .
Wednesday, April 22, 2009
52 - Amyand Hernia & Littre Hernia
A sliding hernia (usually indirect inguinal in location) is a hernia in which a part of the wall of the hernia sac is formed by an intra-abdominal viscus (usually colon, sometimes bladder).
In a Richter hernia, part (rather than the entire circumference) of the bowel wall is trapped.
A Littré hernia is one that contains a Meckel diverticulum.
An Amyand hernia is one that contains the appendix.
51 - Oniomania
Oniomania (from Greek onios = "for sale," mania = insanity) is a medical term for the compulsive desire to shop. Oniomania is the technical term for the compulsive desire to shop, more commonly referred to as compulsive shopping, compulsive buying, shopping addiction or shopaholism. First described by Bleuler in 1915, and then Kraepelin in 1924, as oneomania from the Greek oneomai, to buy, included among other pathological and reactive impulses, compulsive buying went largely ignored for nearly sixty years.
Psychiatrists often call oniomania a disorder, but it has only been accepted as a disorder by the Deutsche Gesellschaft Zwangserkrankungen (German organization for obsessive-compulsive disorders), for several years. In the United States
Only in the past twenty years has specific and persistent inquiry into the disorder occurred. Although the study of compulsive buying is still in its infancy compared with some of its psychological siblings—alcoholism, eating disorders or drug abuse—there is more and more evidence that it poses a serious and worsening problem, one with significant emotional, social, occupational, and financial consequences. As many as 8.9 percent of the American population may be full-fledged compulsive buyers. (Ridgway, et al., 2008), and the problem is fast becoming a global one.
The terms compulsive shopping, compulsive buying, and compulsive spending are often used interchangeably, but the behaviors they represent are in fact distinctly different (Nataraajan and Goff 1992). However, one may buy without shopping or certainly shop without buying. Most current researchers use the term compulsive buying and subscribe to an exceptionally specific definition proposed by McElroy and her colleagues (1994) as follows:
1. Compulsive buying is a maladaptive preoccupation with buying or shopping, or maladaptive buying or shopping impulses or behavior, as indicated by either: frequent preoccupation with buying or impulses to buy that is/are experienced as irresistible, intrusive, and/or senseless, or frequent buying items that are not needed or cannot be afforded or shopping for longer periods of time than intended.
2. The buying preoccupations, impulses, or behaviors cause marked distress, are time-consuming, significantly interfere with social or occupational functioning, or result in financial problems, and they do not occur exclusively during periods of hypomania or mania.
Similar to other compulsive behaviors, sufferers often experience the highs and lows associated with addiction. Victims often experience moods of satisfaction when they are in the process of purchasing, which seems to give their life meaning while letting them forget about their sorrows. Once leaving the environment where the purchasing occurred, the feeling of a personal reward has already gone. To compensate, the addicted person goes shopping again. Eventually a feeling of suppression will overcome the person. For example, cases have shown that the bought goods will be hidden or destroyed, because the person concerned feels ashamed of their addiction and tries to conceal it.
The addicted person gets into a vicious circle that consists of negative emotions like anger and stress, which lead to purchasing something. After the buying is over, the person is eitherregretful or depressed. In order to cope with the feelings, the addicted person resorts to another purchase.
Shopaholism often begins at an early age. Children who experience parental neglect often grow up with low self-esteem because throughout much of their childhood they experienced that they were not important as a person. As a result, they used toys to compensate for their feelings of loneliness. Adults that have depended on materials for emotional support when they were much younger are more likely to become addicted to shopping because of the ongoing sentiment of deprivation they endured as children. During adulthood, the purchase instead of the toy is substituted for affection. Shopaholics are unable to deal with their everyday problems, especially those that alter their self-esteem. Most of the issues in their lives are repressed by buying something.
Social conditions may also play an important role, especially in capitalist societies that are dominated by a consumerist economy where buying is an important part of daily life. Credit cards facilitate the spending of money as well as mail order via catalogues or the Internet. What differentiates oniomania from healthy shopping is the compulsive, destructive nature of the buying.
This disorder is often linked to emotional deprivations in childhood, an inability to tolerate negative feelings, the need to fill an internal void, excitement seeking, excessive dependency, approval seeking, perfectionism, general impulsiveness and compulsiveness, and the need to gain control (DeSarbo and Edwards 1996, Faber et al. 1987, Benson, 2000). Compulsive buying seems to represent a search for self in people whose identity is neither firmly felt nor dependable. Most shopaholics try to counteract feelings of low self-esteem through the emotional lift and momentary euphoria provided by compulsive shopping. These shoppers, who also experience a higher than normal rate of associated disorders—depression, anxiety, substance abuse, eating disorders, and impulse-control disorders—may be using their symptom to self-medicate. Underlying (or at least intensifying) the deeply felt need of problem shoppers is our nationwide outbreak of “affluenza,” the modern American plague of materialism and overconsumption.
The consequences of oniomania, which may persist long after a spree, can be devastating. They may include crushing consumer debt, theft or defalcation of money, defaulted loans, and general financial trouble. Sufferers often come into conflict with the law.
The “smiled upon addiction,” as Catalano and Sonnenberg have called it (1993), is smiled upon in two senses: it is at once a source of wry humor and at the same time a behavior much inflamed by our ever present marketing machinery. As a result, compulsive shopping may be an even greater source of guilt and shame than alcoholism or drug abuse.
In the USA and Canada
Debtors Anonymous
Recovery Connection for Addiction Treatment
Shopping Addicts Only, Yahoo Group
Stopping Overshopping Group Telephone Coaching Program .
Subscribe to:
Comments (Atom)